
Managing MCAS
At present, there is no cure for MCAS. Therefore, the aim of treatment is to reduce the severity of symptoms. There are two main methods for symptom management, the first is through a self-management approach and the second is through the use of medicinal products. Ideally, these two approaches will be combined to achieve the best level of control over the symptoms of MCAS.

Self Management
Avoiding triggers is a key part of managing MCAS and relieving symptoms.
If individuals have been able to identify specific triggers of their symptoms – for example, specific foods or chemicals, exercise or stress – these triggers should be avoided as much as possible to prevent a reaction.
This can include adopting specific diets such as low histamine; controlling blood sugar fluctuations can also be beneficial.
Some people may need to explore a combination of diets depending on their specific triggers, and if this is complicated, seeking help from either a dietician or nutritionist with knowledge of MCAS can be helpful.

Of course, in many cases MCAS triggers are challenging to identify and new triggers may develop over time.
It is not always practical or even possible to avoid every trigger all of the time, particularly in public spaces.
Certain medicines, such as codeine, are also known to trigger MCAS symptoms. Some people with MCAS also benefit from avoiding non-steroidal anti-inflammatory drugs (NSAIDs), such as aspirin or ibuprofen.
Understanding each person’s unique set of triggers can help to better identify which medicines and excipients should be avoided.
You may find it helpful to direct patients to our self-management resource to support them in identifying and managing their triggers.

Medical Management
Several medicines can be used to help alleviate the symptoms of MCAS.
These include mast cell stabilisers; which help restore stability to the mast cell and reduce its reactivity to different triggers, and mediator blockers; which block the release or the effect of different mediators released by the mast cell.
Due to the variation in triggers, mediator release and symptoms across individuals with MCAS, a medical treatment that works for one person may not work for another and the response to treatment is not always predictable.
There is hope for the possibility of personalised MCAS treatment in the future, where prescriptions are tailored to a person’s specific cause, triggers and symptoms, but further research is required to achieve this.

An added complication for the treatment of MCAS arises from the possibility that some drugs (or the additives or preservatives in them) can be triggers for MCAS and this may cause an adverse reaction to a medicine.
This can make it a lengthier and more complicated process to identify a successful medical treatment regimen for someone with MCAS.
However, with a dedicated ‘trial and error’ approach, under careful medical guidance, many people with MCAS are eventually able to find a medical management process that works for them.
The table below provides an overview of some of the different medicines that can be used. The availability of these treatments varies, and some treatments are reserved only for the most severe cases of MCAS.
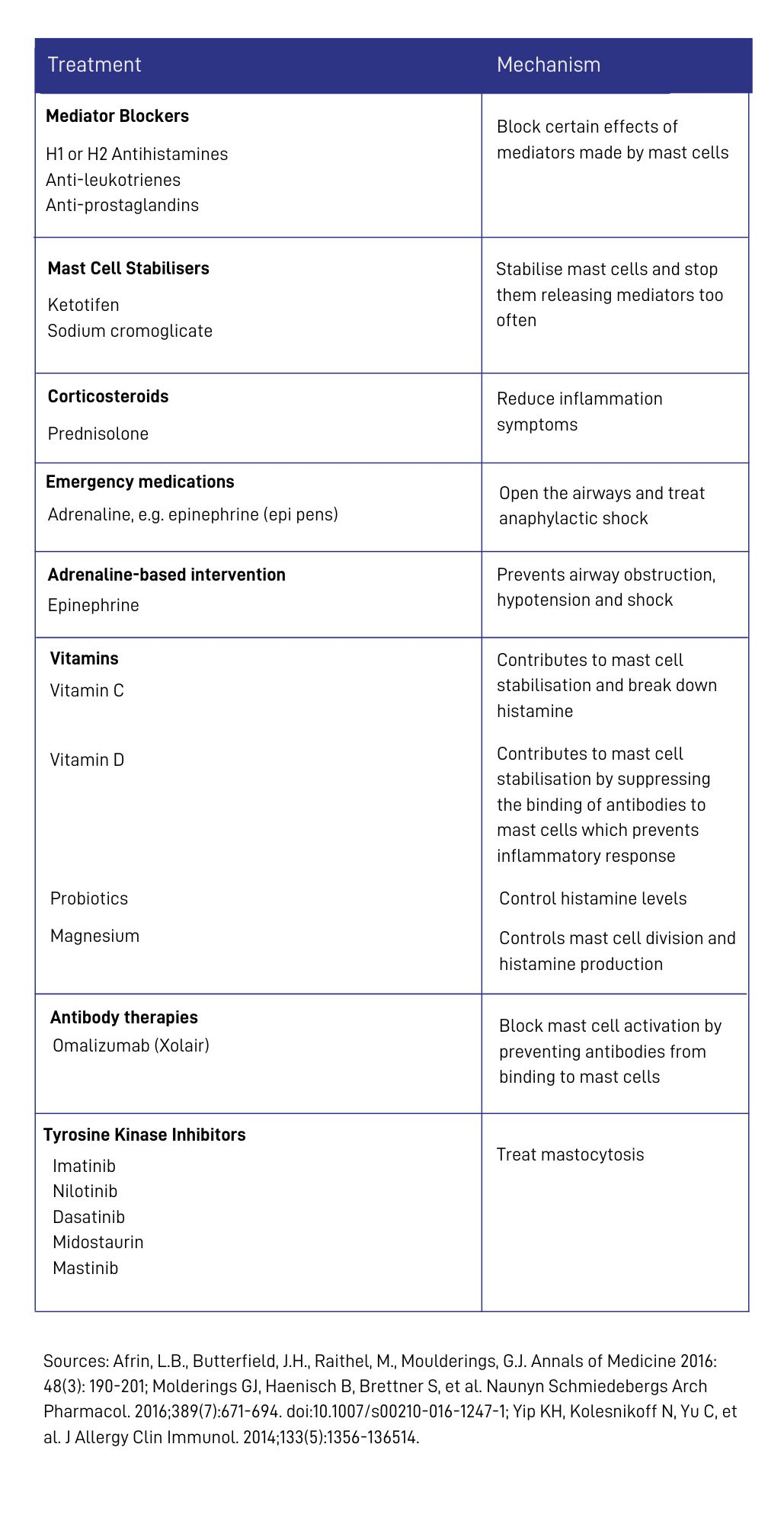
Medicines commonly used to treat MCAS
This table provides an overview of the medicines that have been shown to be effective for managing MCAS. The medicines are divided by whether they impact mast cell mediators or whether if they help to stabilise or inhibit the mast cell itself.
Histamine blockers like H1 and H2s will mitigate the effects of histamine produced by the mast cells. Some medications will manage the effects of other mediators released from mast cells like montelukast, which is a leukotriene blocker and aspirin, which blocks prostaglandins.
Mast call stabilisers which can help prevent mediator release include ketotifen and sodium cromoglycate. Both of these can be prescribed in various forms including capsules and eye drops.
Bioflavonoids such as quercetin and luteolin, and vitamins C and D can also act as mast cell stabilisers.
In Mastocytosis, more than MCAS, anti-body therapies which act as mast cell inhibitors that stop the excessive production of mast cells can be useful.
Medications to support the immune system, like corticosteroids and immunosuppressants may also be prescribed to help reduce inflammation and reduce immune system activity.
Emergency medications include adrenaline, which is used to treat anaphylaxis.
Further reading:
Weiler CR, Austen KF, Akin C, et al. AAAAI Mast Cell Disorders Committee Work Group Report: Mast cell activation syndrome (MCAS) diagnosis and management. J Allergy Clin Immunol. 2019;144(4):883-896.
Castells M, Butterfield J. Mast Cell Activation Syndrome and Mastocytosis: Initial Treatment Options and Long-Term Management. J Allergy Clin Immunol Pract. 2019;7(4):1097-1106.
Become a friend
Sign up to become a Friend of Mast Cell Action so we can keep you up to date on our progress and on how to get involved in our latest campaigns and initiatives.
Donate
Mast Cell Action relies entirely on the generosity of people like you. Please make a donation now and together we can make a difference to those affected by MCAS.







